Chances are you’ve heard of mapping genes to diagnose rare diseases, predict your risk of cancer and tell your ancestry. But to uncover food poisonings?
The nation’s disease detectives are beginning a program to try to outsmart outbreaks by routinely decoding the DNA of potentially deadly bacteria and viruses.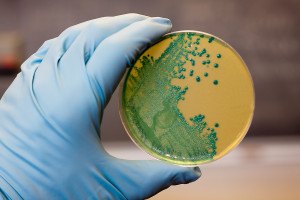
The initial target is listeria, the third-leading cause of death from food poisoning and bacteria that are especially dangerous to pregnant women. Already, the government credits the technology with helping to solve a listeria outbreak that killed one person in California and sickened seven others in Maryland.
“This really is a new way to find and fight infections,” said Dr. Tom Frieden, director of the Centers for Disease Control and Prevention. “One way to think of it is, is it identifying a suspect by a lineup or by a fingerprint?”
Whole genome sequencing, or mapping all of an organism’s DNA, has become a staple of medical research. But in public health, it has been used more selectively, to investigate particularly vexing outbreaks or emerging pathogens, such as a worrisome new strain of bird flu.
For day-to-day outbreak detection, officials rely instead on decades-old tests that use pieces of DNA and aren’t as precise.
Now, with genome sequencing becoming faster and cheaper, the CDC is armed with $30 million from Congress to broaden its use with a program called advanced molecular detection. The hope is to solve outbreaks faster, foodborne and other types, and maybe prevent infections, too, by better understanding how they spread.
“Frankly, in public health, we have some catching up to do,” said the CDC’s Dr. Christopher Braden, who is helping to lead the work.
As a first step, federal and state officials are rapidly decoding the DNA of all the listeria infections diagnosed in the U.S. this year, along with samples found in tainted foods or factories.
It’s the first time the technology has been used for routine disease surveillance, looking for people with matching strains who may have gotten sick from the same source.
If this pilot project works, the CDC says it sets the stage to eventually overhaul how public health laboratories around the country keep watch on food safety, and to use the technology more routinely against other outbreaks.
“Genome sequencing really is the ultimate DNA fingerprint,” said George Washington University microbiologist Lance Price, who uses it to study the spread of antibiotic-resistant bacteria and says the CDC’s move is long overdue.
Foodborne Illness Cases Present Complex Coverage Questions
Especially in foodborne outbreaks, the technology will increase investigators’ ability to nab the right culprit, he said. The faster that happens, the fewer people may get sick.
“This is going to change everything as far as source attribution,” Price added. “Recalls are expensive, the industry doesn’t like them,” and they’ve got to be accurate.
Today’s standard tests sometimes miss linked cases or provide false leads. For example, U.S. officials in 2012 initially thought a salmonella outbreak in the Netherlands, associated with smoked salmon, was linked to cases here. Later sequencing showed the bugs were different.
“The current methods of subtyping salmonella aren’t very good,” said epidemiologist David Boxrud of the Minnesota Department of Health, part of a pilot Food and Drug Administration network that has begun sequencing that germ and certain others when they’re discovered in food. State labs in Arizona, Florida, Maryland, New York, Virginia and Washington also participate.
Sequencing also promises to reveal drug resistance and how virulent a germ is more quickly than today’s tests, and track how it’s spreading from one person to another through tiny genetic changes that act like footprints.
Key to making it work is the computing power of a massive federal database being used to store the gene maps, said Duncan MacCannell, the CDC’s senior adviser for bioinformatics. It’s one thing to analyze bacterial DNA culled from a few dozen sick people during an outbreak, and another to compare samples from thousands.
Until recently, the CDC didn’t have the “tools and approaches to make sense of this much data,” he said.
The listeria project began as officials were investigating some sick Maryland newborns and their mothers. Genome sequencing showed those cases were linked to a California death, helping investigators determine which foods to focus on, said Dr. Robert Tauxe, CDC’s leading foodborne disease sleuth.
Standard tests prompted recall of the FDA’s suspect, a brand of Hispanic-style cheese. Last month, the government announced that sequencing also confirmed listeria from the recalled cheese matched germs from the patients.
“We expect to be able to match more and more of what we find in people to what we find in food,” as the project grows, Tauxe said.
Was this article valuable?
Here are more articles you may enjoy.

 Portugal Rolls Out $2.9 Billion Aid as Deadly Flooding Spreads
Portugal Rolls Out $2.9 Billion Aid as Deadly Flooding Spreads  Tesla Sued Over Crash That Trapped, Killed Massachusetts Driver
Tesla Sued Over Crash That Trapped, Killed Massachusetts Driver  US Will Test Infant Formula to See If Botulism Is Wider Risk
US Will Test Infant Formula to See If Botulism Is Wider Risk  These Five Technologies Increase The Risk of Cyber Claims
These Five Technologies Increase The Risk of Cyber Claims 